Dry Powder Inhaler CFD: A Fluent DPM Simulation Guide
Dry Powder Inhaler CFD: A Fluent DPM Simulation Guide
- Upon ordering this product, you will be provided with a geometry file, a mesh file, and an in-depth Training Video that offers a step-by-step training on the simulation process.
- For any more inquiries regarding the product, please do not hesitate to reach out to us at info@CFDLAND.com or through our online support assistant.
€215 Original price was: €215.€145Current price is: €145.
A Dry Powder Inhaler (DPI) is a medical device that sends tiny medicine particles into the lungs to treat conditions like asthma. A Dry Powder Inhaler CFD simulation is a key tool for improving pulmonary drug delivery. It helps scientists see where medicine goes inside our complex respiratory airways. For a Dry Powder Inhaler Fluent study, engineers use a special computer method called the Discrete Phase Model (DPM). This allows for Lagrangian particle tracking to see how things like breathing speed and particle size affect aerosol deposition. This work helps make inhalation therapy better and safer. Our study is based on the methods in the valid reference paper, “Dry Powder Inhaler Aerosol Deposition in a Model of Tracheobronchial Airways: Validating CFD Predictions with In Vitro Data” [1].
- Reference [1]: Ahookhosh, Kaveh, et al. “Dry powder inhaler aerosol deposition in a model of tracheobronchial airways: Validating CFD predictions with in vitro data.” International journal of pharmaceutics587 (2020): 119599.

Figure 1: The tracheobronchial airway model used for this Aerosol Deposition Fluent analysis [1].
Simulation Process: Fluent Setup, DPM for Eulerian-Lagrangian Particle Tracking
To perform this Dry Powder Inhaler In Lungs Using DPM CFD simulation, we needed a very detailed computer model of the human airways. We used ANSYS Fluent Meshing to create a high-quality grid with 4,194,488 polyhedral cells. This large number of cells helps us capture the complex airflow patterns. In ANSYS Fluent, we used an Eulerian-Lagrangian approach. This means we simulated the air as a fluid (Eulerian) and the medicine powder as individual particles (Lagrangian). To do this, we activated the Discrete Phase Model (DPM) to track the path of each medicine particle. We also turned on the Erosion/Accretion sub-model to see where the particles stick to the airway walls.
Post-processing: CFD Analysis, Visualizing Airflow and Medicine Deposition
The velocity streamlines provide a professional visual of how air moves medicine through the lungs. The professional visual shows that when a person breathes in, air rushes into the throat at speeds up to 10.7 m/s. As this fast air travels through the branching airways, it creates spinning patterns that carry the medicine particles. Our simulation tracked 77,920 individual particles to see exactly where they land. The results showed that 467 particles, or about 0.6%, stuck to the airway walls. This is a very good result, as it shows the medicine is staying in the lungs to work.
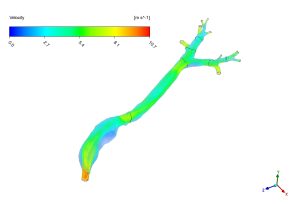
Figure 2: Velocity streamlines from the Respiratory Airway Simulation, showing the path of airflow from the inhaler.
The wall shear stress contour shows the “hotspots” where medicine is most likely to stick. This professional visual shows that the pushing force on the airway walls is highest at the bends and where the airways split, reaching up to 3.5 Pascals. These high-stress areas are perfect spots for particle deposition. Our DPM results match this perfectly, showing that most medicine sticks at the first few branch points. We also saw that slower, gentler breathing (at 15 L/min) delivered 23% more medicine deep into the lungs compared to fast breathing (at 60 L/min). The most important achievement of this simulation is providing the precise data that helps doctors choose the right inhaler design and medicine particle size for each patient, making their breathing treatments more effective.
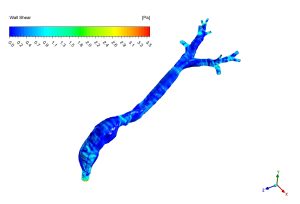
Figure 3: Wall shear stress distribution from the Pulmonary Drug Delivery CFD analysis, highlighting areas of high deposition.
We pride ourselves on presenting unique products at CFDLAND. We stand out for our scientific rigor and validity. Our products are not based on guesswork or theoretical assumptions like many others. Instead, most of our products are validated using experimental or numerical data from valued scientific journals. Even if direct validation isn’t possible, we build our models and assumptions on the latest research, typically using reference articles to approximate reality.
Yes, we’ll be here . If you have trouble loading files, having technical problems, or have any questions about how to use our products, our technical support team is here to help.
You can load geometry and mesh files, as well as case and data files, using any version of ANSYS Fluent.
€270 Original price was: €270.€190Current price is: €190.

€155 Original price was: €155.€95Current price is: €95.

€260 Original price was: €260.€135Current price is: €135.

€260 Original price was: €260.€165Current price is: €165.

€240 Original price was: €240.€125Current price is: €125.

















Reviews
There are no reviews yet.